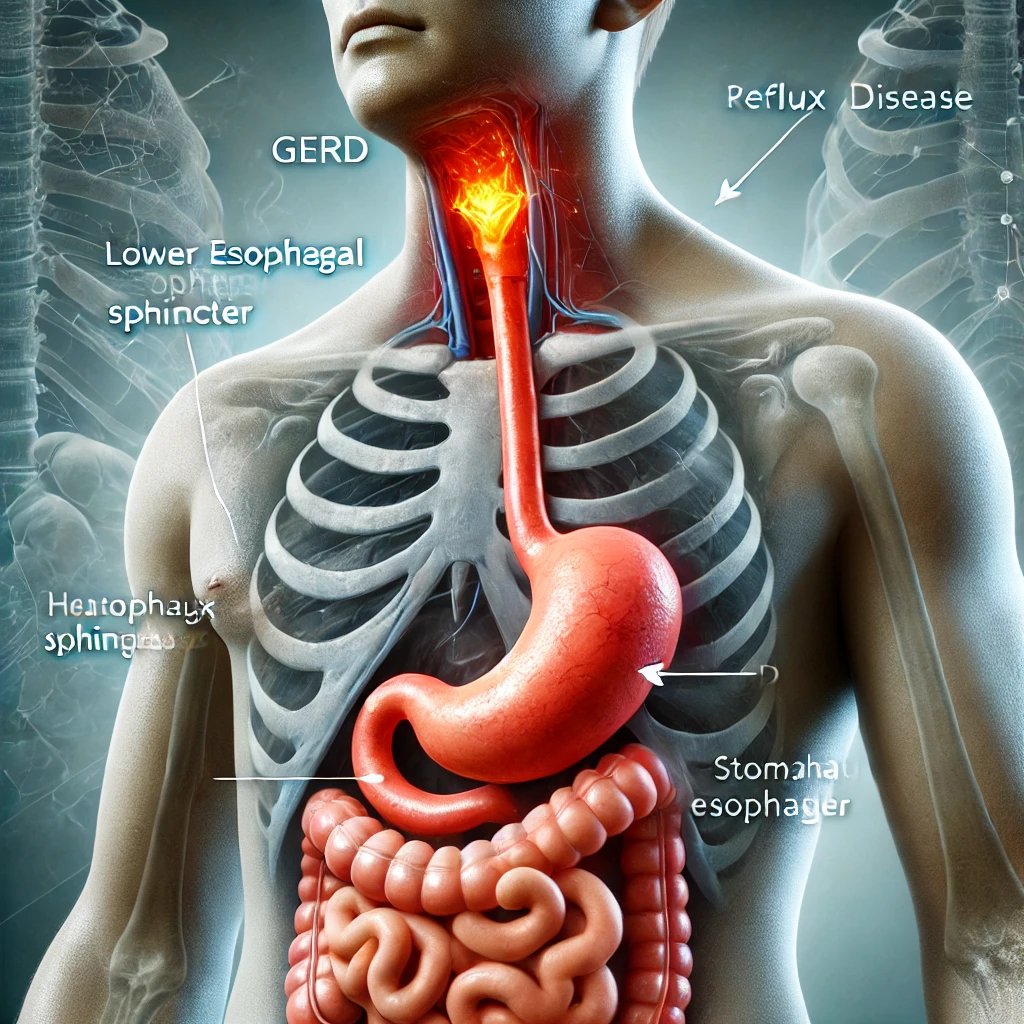
Gastroesophageal Reflux Disease (GERD) is a chronic digestive disorder characterized by the frequent backflow of stomach acid or bile into the esophagus, the tube connecting the mouth to the stomach. This occurs when the lower esophageal sphincter (LES), a ring of muscle that acts as a valve between the esophagus and stomach, weakens or relaxes abnormally. The repeated exposure of the esophageal lining to stomach acid can cause irritation, inflammation, and potentially lead to complications if left untreated. This is diagnosed when acid reflux occurs more than twice a week or causes significant symptoms or damage to the esophagus. Common symptoms include heartburn, regurgitation, and difficulty swallowing, though it can also present with atypical symptoms like chronic cough or chest pain. Manage Gastroesophageal Reflux Disease is essential before body damage and further complications and embrace a future free from discomfort.
Gastroesophageal Reflux Disease (GERD): Introduction
Gastroesophageal Reflux Disease (GERD) is a common yet often misunderstood condition that affects millions of people worldwide. If you’ve ever experienced the burning sensation in your chest after eating, or felt like food is stuck in your throat, you might already be familiar with GERD. This chronic digestive disorder occurs when stomach acid frequently flows back into the esophagus—the tube connecting your mouth to your stomach. Over time, this backwash can irritate the lining of the esophagus, leading to discomfort and potentially serious complications.
Understanding Gastroesophageal Reflux Disease (GERD) is essential for maintaining long-term health. While occasional heartburn is normal, persistent symptoms could indicate GERD, which requires proper attention. Left untreated, GERD can significantly impact your quality of life, causing sleep disturbances, dietary restrictions, and even more severe conditions like Barrett’s esophagus or esophageal cancer. In this article, we’ll dive deep into what causes GERD, its symptoms, risk factors, treatment options, and lifestyle changes that can help manage it effectively.
If you’re tired of heartburn ruining your meals or interfering with your daily routine, this guide on Gastroesophageal Reflux Disease (GERD) will provide valuable insights to empower you to take control of your digestive health. Let’s explore everything you need to know about this condition so you can make informed decisions about your well-being.
The Science Behind Gastroesophageal Reflux Disease (GERD): How Does It Happen?
To fully grasp Gastroesophageal Reflux Disease (GERD), it’s important to understand the underlying mechanisms at play. At the heart of GERD lies the lower esophageal sphincter (LES), a ring of muscle located where the esophagus meets the stomach. The LES acts as a valve, opening to allow food to pass into the stomach and closing to prevent stomach contents from flowing back up. When the LES weakens or relaxes abnormally, stomach acid can escape into the esophagus, triggering the hallmark symptoms of GERD.
Several factors contribute to this malfunctioning of the LES. Obesity, smoking, and certain medications can all weaken the LES, making it easier for acid reflux to occur. Additionally, consuming large meals or lying down immediately after eating can increase pressure on the stomach, forcing acid upward. Some individuals may also have a naturally weaker LES due to genetic predisposition or structural abnormalities such as a hiatal hernia.
Understanding how Gastroesophageal Reflux Disease (GERD) develops not only helps identify its root causes but also highlights why managing triggers and adopting preventive measures are critical. By addressing these contributing factors, you can reduce the frequency and severity of GERD episodes. Later in this article, we’ll discuss specific strategies to strengthen the LES and minimize acid reflux, ensuring you stay informed about tackling Gastroesophageal Reflux Disease (GERD) head-on.
Common Symptoms of Gastroesophageal Reflux Disease (GERD): Is It More Than Just Heartburn?
When discussing Gastroesophageal Reflux Disease (GERD), most people immediately think of heartburn—a sharp, burning pain behind the breastbone. However, GERD encompasses far more than just this classic symptom. Recognizing the full spectrum of symptoms is crucial for early diagnosis and effective management of the condition.
In addition to heartburn, GERD sufferers often experience regurgitation, where sour or bitter-tasting liquid rises into the mouth. Difficulty swallowing (dysphagia) is another red flag, signaling potential damage to the esophagus. Less obvious signs include chronic cough, hoarseness, sore throat, and even asthma-like symptoms caused by acid irritating the airways. These less common manifestations can sometimes lead to misdiagnosis, underscoring the importance of understanding Gastroesophageal Reflux Disease (GERD) comprehensively.
If you’re experiencing any combination of these symptoms regularly, it’s vital to consider whether GERD might be the culprit. Early intervention can prevent complications and improve your overall quality of life. As we delve deeper into Gastroesophageal Reflux Disease (GERD), keep these symptoms in mind—they serve as key indicators that warrant further investigation.
Risk Factors and Triggers: Who’s Most Likely to Develop Gastroesophageal Reflux Disease (GERD)?
Certain lifestyle choices and medical conditions significantly elevate the risk of developing Gastroesophageal Reflux Disease (GERD). Identifying these risk factors and triggers is a pivotal step toward prevention and effective management. For instance, obesity places extra pressure on the abdomen, pushing stomach contents upward and weakening the LES. Similarly, smoking reduces LES functionality and increases acid production, creating a perfect storm for GERD development.
Dietary habits also play a major role in Gastroesophageal Reflux Disease (GERD). Consuming fatty, fried, or spicy foods, along with beverages like coffee, alcohol, and carbonated drinks, can exacerbate symptoms. Even seemingly harmless habits, such as eating large meals or lying down shortly afterward, can trigger acid reflux. Pregnant women are particularly susceptible due to hormonal changes and increased abdominal pressure.
Knowing who is most vulnerable to Gastroesophageal Reflux Disease (GERD) allows for proactive steps to mitigate risks. Whether through weight loss, quitting smoking, or modifying your diet, small changes can yield significant improvements. Keep reading to learn how these adjustments tie into broader strategies for combating Gastroesophageal Reflux Disease (GERD).
Complications of Untreated Gastroesophageal Reflux Disease (GERD): Why Early Intervention Matters
Ignoring the warning signs of Gastroesophageal Reflux Disease (GERD) can have serious consequences. Over time, repeated exposure to stomach acid damages the esophageal lining, leading to inflammation known as esophagitis. Without proper treatment, this inflammation can progress to more severe Complications of Gastroesophageal Reflux Disease (GERD) including ulcers, strictures (narrowing of the esophagus), and Barrett’s esophagus—a precancerous condition linked to an increased risk of esophageal cancer.
Beyond physical health, untreated GERD takes a toll on mental and emotional well-being. Chronic pain and disrupted sleep patterns can result in fatigue, anxiety, and depression. Moreover, dietary restrictions imposed by GERD may limit social interactions and enjoyment of meals, further impacting quality of life.
Early intervention is key to preventing these outcomes. By recognizing the dangers associated with unmanaged Gastroesophageal Reflux Disease (GERD), you can prioritize timely diagnosis and treatment. Stay tuned as we explore diagnostic methods and treatment options designed to combat Gastroesophageal Reflux Disease (GERD) effectively.
Diagnosing Gastroesophageal Reflux Disease (GERD): How Do Doctors Confirm It?
Accurate diagnosis is the cornerstone of managing Gastroesophageal Reflux Disease (GERD). Physicians use a variety of tests to confirm the presence of GERD and rule out other conditions with similar symptoms. Endoscopy, one of the most common procedures, involves inserting a flexible tube with a camera down the throat to examine the esophagus and stomach for signs of irritation or damage.
Other diagnostic tools include pH monitoring, which measures acid levels in the esophagus over 24 hours, and barium swallow X-rays to detect structural issues like hiatal hernias. If you suspect you have Gastroesophageal Reflux Disease (GERD), don’t hesitate to seek medical advice. Early detection ensures prompt treatment, reducing the likelihood of complications.
This section has provided insight into diagnosing Gastroesophageal Reflux Disease (GERD), emphasizing the importance of professional evaluation. Moving forward, we’ll discuss treatment options tailored to address the unique needs of GERD patients.
Treatment Options for Gastroesophageal Reflux Disease (GERD): Finding Relief That Works for You
Managing Gastroesophageal Reflux Disease (GERD) requires a personalized approach, combining medication, lifestyle modifications, and, in some cases, surgical interventions. Over-the-counter remedies like antacids offer quick relief by neutralizing stomach acid, while H2 blockers and proton pump inhibitors (PPIs) provide longer-lasting results by reducing acid production.
For those with severe or refractory GERD, advanced treatments such as fundoplication surgery or the LINX device may be recommended. These options aim to reinforce the LES and prevent acid reflux. Regardless of the chosen method, finding the right solution depends on understanding the nuances of Gastroesophageal Reflux Disease (GERD) and working closely with healthcare providers.
As we continue exploring Gastroesophageal Reflux Disease (GERD), remember that effective treatment begins with accurate diagnosis and commitment to sustainable lifestyle changes. Keep reading for practical tips to incorporate into your daily routine.
Lifestyle Changes to Manage Gastroesophageal Reflux Disease (GERD) Naturally
Adopting healthy habits is one of the most effective ways to manage Gastroesophageal Reflux Disease (GERD). Simple adjustments, such as avoiding trigger foods, eating smaller portions, and staying upright for at least two hours after meals, can make a world of difference. Incorporating regular exercise and maintaining a healthy weight also alleviates pressure on the abdomen, reducing the risk of acid reflux.
Mindful eating practices, such as chewing thoroughly and sipping water instead of gulping, promote better digestion and minimize GERD symptoms. Quitting smoking and limiting alcohol consumption further support LES function and overall digestive health. Embracing these lifestyle changes not only addresses Gastroesophageal Reflux Disease (GERD) but fosters holistic wellness.
By focusing on natural solutions, you can take charge of your GERD journey. Continue reading to uncover additional strategies for living well with Gastroesophageal Reflux Disease (GERD).
Living Well with Gastroesophageal Reflux Disease (GERD): Empowering Yourself for Long-Term Health
Living with Gastroesophageal Reflux Disease (GERD) doesn’t mean sacrificing your quality of life. With the right knowledge and tools, you can thrive despite the challenges posed by this condition. From understanding its causes to implementing effective treatments and lifestyle changes, this article has equipped you with the resources needed to tackle Gastroesophageal Reflux Disease (GERD) confidently.
Remember, early action and consistent care are your best allies in managing GERD. Don’t let Gastroesophageal Reflux Disease (GERD) define your life—start taking steps today to reclaim your health and happiness.
Conclusion: Your Path to Better Digestive Health Starts Now
In conclusion, Gastroesophageal Reflux Disease (GERD) is a manageable condition that demands attention and proactive measures. By educating yourself about its causes, symptoms, and treatments, you’re already on the path to better digestive health. Take control of your GERD journey today, and embrace a future free from unnecessary discomfort.